Does this sound familiar? You wake up already exhausted. You’re struggling to keep your eyes open. You can barely concentrate on your work. Every conversation feels like climbing a mountain, and it’s causing conflicts with your colleagues and the people you love. By evening, you find yourself scrolling mindlessly through Netflix or whatever streaming platform you use until the early hours because sleep just feels impossible. And meanwhile, every muscle, every joint, every bone in your body aches like you’ve run a marathon – except you haven’t moved from your desk chair all day.
If that sounds like you, I want you to know something important: you’re not alone. Not even close.
The numbers are staggering. Fatigue is one of the most common symptoms people report to their primary care doctors. Studies estimate that chronic fatigue, the kind that lasts for months, affects somewhere between 7 and 10% of adults worldwide.
What’s even more concerning is what we’ve seen since 2020. Workplace absences and long-term sickness leave have climbed dramatically in many countries. And here’s the thing: this isn’t about one simple problem. Research shows that persistent exhaustion rarely has a single cause. Instead, it’s this complicated web where disrupted sleep tangles with metabolic changes, hormonal shifts, pain from our sedentary lifestyles, and psychological stress – all feeding into each other in ways doctors are only beginning to understand.
The truth is far more complex than the simple “just stress” explanation.
Today, we’re going to dive deep into what’s really going on in your body when you feel this persistent exhaustion. And I promise you, by the end of this article, you’ll understand things about your health that most people never learn.
Before we get started, I need to mention something important. Everything we discuss here is for educational purposes only. It doesn’t replace medical advice from your doctor. Think of this as information to help you have better conversations with your healthcare provider.
The Coffee Machine Analogy
Let me start with something simple – a filter coffee machine. Just think about that basic setup for a moment. When it breaks down and starts giving you cold, brown liquid instead of hot coffee, you can usually figure out the problem pretty quickly, right? The heating element failed. Simple machine, simple solution. You either replace the part or get a new machine.
Now imagine one of those high-tech coffee machines loaded with electronics, multiple brewing options, smart connectivity, the whole nine yards. When this machine malfunctions, troubleshooting becomes exponentially more difficult. You might spend hours trying to locate the root cause among dozens of interconnected systems. Is it the processor? The sensor? The software? A connection issue? It could be anything.
Here’s the thing: your body operates like that complex coffee machine, except it’s infinitely more sophisticated. I’m not exaggerating when I say it’s arguably the most intricate system in the known universe. You’ve got countless interconnected processes working in harmony every single second of every day.
And here’s what’s really fascinating: when one system begins to struggle, others step in to compensate. For minor issues lasting a few days or weeks, this backup system works beautifully. Your body is incredibly resilient.
But what happens when small problems persist for months or years? That’s when things start to break down in ways that seem mysterious and frustrating.
Remember your body isn’t a simple machine – it’s a living network. When one part struggles, others step in to compensate. But if the imbalance lasts too long, the whole system starts to strain.
Peter’s Story: The Hidden Chain Reaction
Let me tell you a story that illustrates this perfectly. Let’s imagine Peter – a 50-year-old bank employee who spends his days sitting at a customer service desk. After eight hours of solving other people’s problems, he drives home and collapses on his couch to watch the news. His only real movement each day is the walk from his front door to his car. That’s it.
After several years of this routine, Peter starts to develop knee pain that gradually gets worse – eventually leaving him limping. On top of that, he often has lower back pain and has had a few bouts of sciatica. The pain in his knee becomes so bad that he can barely walk to his car.
Now, most people – including Peter – would assume this is just about his knee. Maybe arthritis, maybe an old injury finally catching up with him. But here’s where it gets interesting, and where most people miss the real story.
Peter’s knee pain didn’t just appear out of nowhere. It’s actually the final domino in a chain reaction that started months earlier.
Think of your body like a tent held up by several poles. When one pole moves or tilts, the whole tent shifts to stay balanced. Your body works the same way – if one part is out of alignment, everything else adjusts to keep you steady.
Peter’s long hours of sitting created a ripple effect throughout his entire body. His core muscles – the ones that should be holding him upright -gradually became weak and lazy from lack of use. When your core can’t do its job, other muscles have to pick up the slack. Some muscles started working overtime, becoming tight and overworked. Others got stretched out and weak.
Over time, this shifted how his hips, knees, and ankles lined up. By the time Peter felt that first twinge in his knee, his whole body had already been quietly reorganizing itself for months.
Now, Peter’s story is illustrative. Only a qualified medical professional can determine the cause of symptoms like these and recommend appropriate care. But the principle here is backed by solid research.
Back in 2019, researchers Jéssica Kirsch Micheletti and her colleagues at Denmark’s National Research Centre for the Working Environment did something remarkable. They analyzed data from more than 10,000 working adults and found something that should make all of us sit up and pay attention: the longer people sat, the more pain they experienced – and not just in their backs or necks. We’re talking knees, shoulders, hips. The study showed that sitting essentially amplifies pain throughout your entire body. The more you sit, the worse it gets.
A couple years later, in 2021, Francis Q.S. Dzakpasu and his team conducted a massive review of multiple studies – both workplace and non-workplace settings. Their findings? The connection between sitting and pain held up across the board. It didn’t matter how old you were or what job you had. But here’s the hopeful part: they also found that even moderate physical activity could meaningfully reduce this risk.
Then, just last year in 2024, Goyal and colleagues published a comprehensive review that really connected all the dots. They showed that prolonged sitting isn’t just a musculoskeletal problem – it’s wreaking havoc on your entire system. We’re talking metabolic dysfunction, fatigue, even cognitive decline. This modern “chair-bound” lifestyle? It’s contributing directly to the kind of whole-body exhaustion and discomfort that people like Peter experience every single day.
When you put all this research together, the message is crystal clear: chronic inactivity doesn’t just hurt one joint or one muscle. It creates this cascading effect of strain throughout your entire body. And that’s exactly why pain and fatigue so often show up together – they’re both your body’s way of signaling that something deeper is out of balance.
This is just one example of the hidden connections running through your body. And here’s what I want you to understand: there are dozens of these invisible chains linking seemingly unrelated symptoms to their true causes. Throughout our articles, we’ll reveal these secret connections so you can understand what’s really happening in your body and make changes that will actually fix the problem – not just mask the symptoms.

Peter’s story reminds us that pain and fatigue are rarely isolated problems. They’re often signals from deeper patterns – tiny misalignments that echo through the entire body. Understanding the chain reaction is the first step toward breaking it.
When Your Body Runs Out of Backup Plans
Our bodies are remarkably resilient. They’re constantly making these tiny micro-adjustments to keep us functioning despite our less-than-ideal habits. Initially, these compensations work so well that we don’t notice anything wrong.
The deterioration happens gradually, like watching a plant slowly wilt. You don’t notice the change from day to day, but if you compare today to six months ago, you’d see a dramatic difference.
We often dismiss those early warning signs, telling ourselves we’re just going through a rough patch that will pass. “I just need to get through this busy season at work.” “Once the kids are back in school, things will settle down.” “After this project is done, I’ll take better care of myself.”
But eventually, our body’s compensatory mechanisms become overwhelmed. And you know what’s really frustrating? The breakdown often happens suddenly, at the most inconvenient moment possible – right before an important exam, a major presentation, or a long-awaited vacation.
Have you ever noticed this? How you seem to get sick just before holidays or significant events? This isn’t a coincidence. It’s not Murphy’s Law. Your body has been running on reserve power for so long that when you finally allow yourself to relax, it essentially crashes.
The stress hormones that were keeping you upright suddenly drop, and your suppressed immune system can no longer fight off that virus you’ve been carrying around. This phenomenon is so common that researchers have actually documented it extensively. A 2020 study by Mathieu Nollet and colleagues at the University of Groningen in the Netherlands found that sleep deprivation and stress create this reciprocal relationship where each condition worsens the other, creating a downward spiral that becomes increasingly difficult to break.
Chronic exhaustion isn’t a single event – it’s an accumulation of tiny imbalances over time. Your body keeps adapting… until it can’t. Recognizing those early signs means you can act before the crash.
The Exhaustion Epidemic: Recognizing the Signs
So let’s talk about what chronic exhaustion really looks like. Because the symptoms extend far beyond just feeling tired. I want to be clear here – these are general signs that researchers have associated with fatigue syndromes, but they’re not diagnostic. Similar symptoms can result from a wide range of unrelated causes. Always speak to a healthcare provider before drawing conclusions.
But let me paint you a picture of what this condition really looks like in daily life, because I think you’ll recognize some of these patterns.
Five Physical Symptoms:
First, there’s unrefreshing sleep. You spend 8 to 10 hours in bed but wake up feeling like you haven’t slept at all. Or maybe you consistently sleep less than 7 hours and just can’t seem to get more.
Second, there’s chronic pain. Headaches, muscle aches, back pain, stomach problems – they become your constant companions. You wake up with them, you go to bed with them.
Third, digestive issues are really common too. Alternating between constipation and diarrhea, often with bloating and discomfort, maybe heartburn thrown in there.
Fourth, you catch every cold that goes around, and you take longer to recover than you used to. Your immune system is just tired.
Fifth, and here’s a really frustrating one: exercise intolerance. Instead of helping you feel better, physical activity makes you feel worse—sometimes for several days. This really messes with people because we all know exercise is supposed to be good for us, right?
Beyond Physical: Cognitive, Emotional and Behavioral Signs
However, that’s not all. The problems go beyond physical conditions, touching your cognitive functions, emotions, and behaviors:
First, brain fog is a big one. Simple tasks take twice as long. You’re easily distracted. You forget basic information. You walk into a room and have no idea why you went there.
Second, your emotions might swing quickly and feel hard to control. You might feel overwhelmed, anxious, or unusually sensitive, even in situations that wouldn’t normally affect you so strongly.
Third, there’s this pervasive sense of hopelessness – like nothing will improve – accompanied by low self-esteem. Everything feels more overwhelming than it should.
Next, you need large amounts of coffee just to function, followed by energy drinks to make it through the day. You’re basically running on caffeine and willpower.
What’s more, you start avoiding friends and family because you just lack the energy for social interaction. Activities you once enjoyed feel impossible to pursue.
Sleep? Forget about it. You spend hours in the evening replaying the day’s events and worrying about tomorrow, which makes a good rest even more elusive.
And lastly, basic self-care feels like monumental tasks, not to mention taking time to prepare a nutritious meal for yourself.
If you recognize multiple patterns here, it’s still not too late to regain control of your life. The knowledge in this article can help you have a better conversation with your physician, who can conduct appropriate evaluations and prescribe personal treatment.

The Hidden Connections: The Sleep and Weight Gain Link
Now, here’s where most people get frustrated with general health advice that you can find on the internet. They try to fix one thing at a time and wonder why nothing gets better. The truth is, everything in our bodies is connected in ways that aren’t obvious at first glance.
Let me give you a perfect example that might surprise you: the connection between poor sleep and weight gain.
Of course, poor sleep makes you tired – that’s no surprise. But what’s happening inside your body is much more dramatic than that.
When you consistently sleep less than seven hours a night, your body starts playing tricks on you. It’s like your internal control system goes haywire.
Imagine your body has two main hunger messengers. One says “I’m hungry!” and the other says “I’m full, stop eating!” When you don’t get enough sleep, the “I’m hungry!” messenger gets louder and more demanding, while the “I’m full!” messenger practically whispers.
There’s this groundbreaking study from the University of Chicago – published by Karine Spiegel, Rachel Leproult, and Eve Van Cauter back in 2011 -that found people who don’t sleep enough have their hunger hormones completely reversed. The hormone that makes you crave food – especially sugary, fatty foods – shoots up, while the hormone that tells you to stop eating drops way down. It’s like your body is sabotaging your willpower from the inside.
But it gets worse. Their research showed that poor sleep also messes with your body’s ability to process sugar properly. This means that even if you eat the same foods, your body is more likely to store them as fat instead of using them for energy. The evidence linking insufficient sleep to increased risk of weight gain was already clear even a decade ago.
This explains why you find yourself standing in the kitchen at 10 PM, eating ice cream straight from the box even though you had dinner two hours ago. It’s not because you lack willpower – it’s because your sleep-deprived body is literally screaming for food, and your ability to say “no” has been chemically suppressed.
What’s particularly eye-opening is how common this problem has become. Studies by Matthew Rogers and colleagues published in Diabetes/Metabolism Research and Reviews in 2024 show that people who chronically don’t get enough sleep are significantly more likely to become obese. It’s not just about being tired – it’s about how sleep loss rewires your entire relationship with food.

Everything in your body is connected. Sleep affects hunger, hunger affects stress, and stress affects sleep. Once you see the links, you realize fatigue isn’t random – it’s a map you can learn to read.
The Four Pillars Framework
Over the past few years, I’ve been digging through research from all over – nutrition, exercise science, sleep studies, psychology. And the more I read, the more I saw these patterns: when one system struggles, other systems start to falter. The catch is that most research zooms in on just one part of the picture.
That’s what inspired me to put together what I call the Four Pillars framework. It’s basically my way of connecting the dots – bringing those scattered findings into one picture so it’s easier to understand how the body actually works as a whole.
Now, just so we’re clear, this framework is for educational use only. It’s not a diagnostic or clinical tool.
The Four Pillars framework is my attempt to synthesize this research into a coherent model that makes these hidden connections visible and understandable.
So here’s the basic idea: I’ve identified four basic areas that form the foundation of feeling good in daily life. Think of these as the four legs of a chair. When they’re all strong and balanced, you feel stable and energized. But if one leg is weak or broken, the whole thing becomes unstable.
And here’s what makes this really challenging: these connections aren’t always obvious. When something goes wrong in one area, it creates a chain reaction that ripples through the others. It’s like pulling one thread in a sweater – suddenly, the whole thing starts to unravel.
That’s why working on just one thing – like starting a diet or trying to get more sleep – often doesn’t work long-term. The weakness in the other areas keeps pulling you back down.
Let me walk you through each pillar and show you how they’re interconnected.
Pillar 1: FUEL – Nutrition and General Health
This is all about what you put into your body and your underlying health conditions. We’re talking about processed foods and sugar crashes that leave you drained. We’re talking about inflammation that your body has to constantly fight. We’re talking about hidden hormonal cycles that regulate your energy throughout the day. And hidden health conditions like thyroid dysfunction, insulin resistance, or gut health issues that can silently drain your energy. Plus, those essential nutrients your body desperately needs – but isn’t getting.
Pillar 2: MOVEMENT – Your Physical Foundation
This pillar covers what I call “the sitting disease” – those postural problems and muscle weakness that develop when we don’t move enough. Pain patterns that create chronic tension and movement dysfunction. Training mistakes people make when they go from zero to hero in one night, trying to fix everything with one intense workout.
Pillar 3: MIND – Mental and Emotional Health
This includes your thought patterns – those negative thinking loops and rumination that keep you up at night. Your social connections – or lack thereof. Isolation, the comparison trap, relationship health. Your stress response – how chronic stress impacts your body and your coping mechanisms. And here’s something really important: living without purpose. When you don’t have a sense of meaning or direction, it drains your energy in ways that are hard to describe.
Pillar 4: RHYTHM – Daily Habits and Circadian Health
This pillar covers your sleep hygiene and circadian disruption. Your digital habits – social media addiction and screen time impact. And time management – procrastination, feeling overwhelmed, productivity issues.
Now, here’s the key insight: these four areas function like a house’s foundation. When one area is weak, the others must work overtime to compensate. Eventually, they all may start to decline.
But here’s the hopeful part, and I really want you to hear this: when one area strengthens, it naturally supports the others. Better sleep is associated with healthier eating patterns. Regular movement correlates with improved sleep quality. Reduced stress is linked to enhanced immune function. Strong relationships provide emotional support that makes all the other behavioral changes easier.
This structure helps you organize how you think about these connections. Taking time to calmly reflect on and analyze your situation can be an excellent starting point for presenting your concerns to your doctor in a clear, structured way.
The same connections that made the problem complicated are what make recovery possible once you understand how to work with them.
We’ve uncovered the four foundations of lasting energy: fuel, movement, mind, and rhythm. Strengthen one, and the others follow. That’s where recovery begins – not in perfection, but in balance.
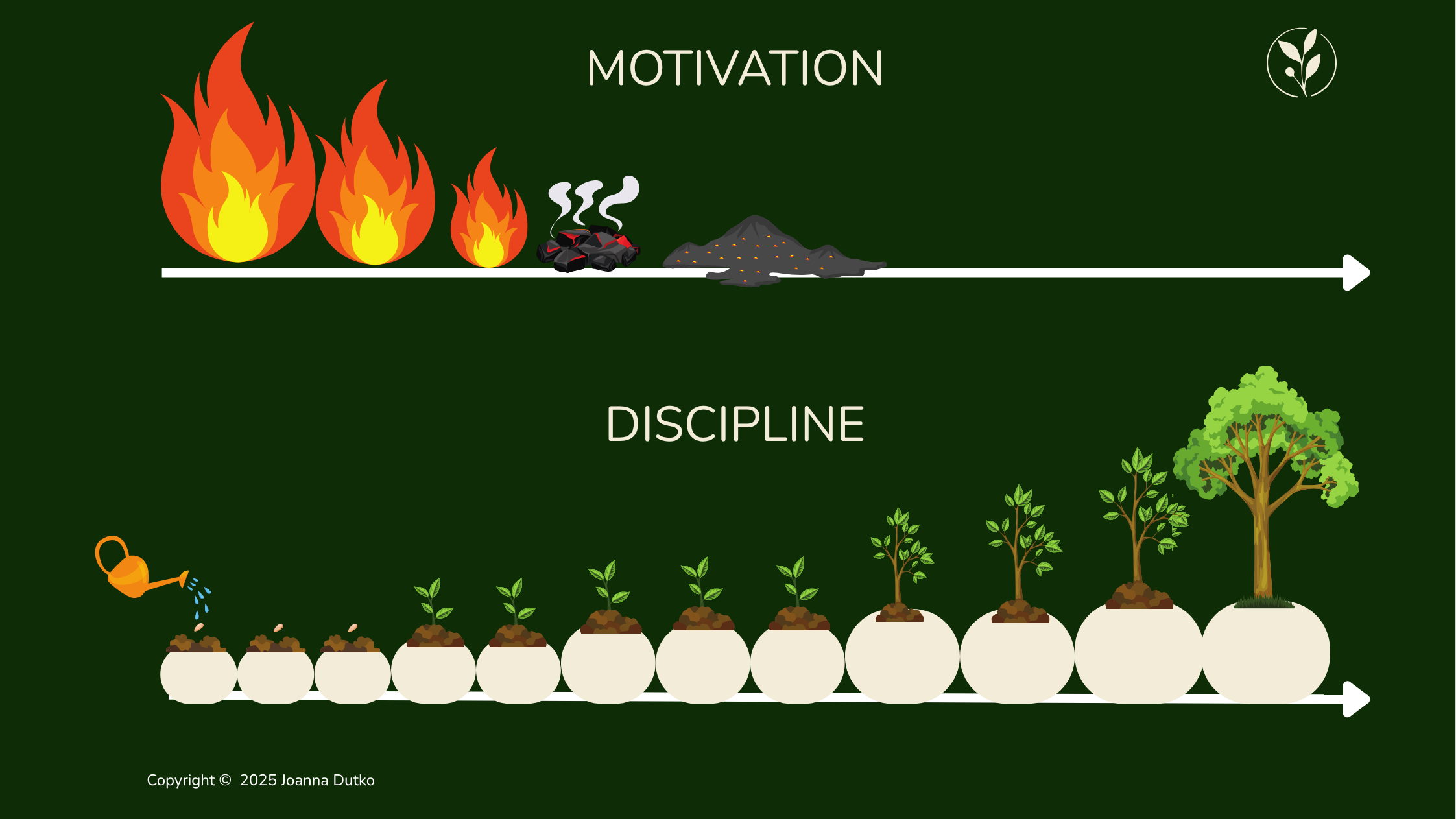
Why Quick Fixes Don’t Work
Okay, I’m going to be really honest with you here. The uncomfortable truth is that there are no shortcuts to recovering from persistent fatigue and low well-being.
I know that’s not what you want to hear. We all want the magic pill, the one weird trick, the quick fix. But here’s the thing: the very mindset that seeks quick fixes – the same one that led to taking shortcuts with sleep, nutrition, and self-care – is part of what created this problem in the first place.
This doesn’t mean recovery is impossible. It absolutely doesn’t. It just means it requires a systematic approach that addresses multiple pillars simultaneously.
Think of it like renovating a house. You can’t just paint over water damage and expect it to look good. You need to fix the leak, repair the structural damage, and then address the cosmetic issues. If you just paint over the water damage, it’s going to come back. It might look okay for a week or two, but eventually, you’re going to see those stains bleeding through again.
The good news – and there really is good news here – is that once you begin addressing these interconnected issues, improvements in one area naturally support improvements in others. The same interconnectedness that made the problem complex also makes recovery more effective once you understand how to work with it rather than against it.
Your Path Forward
So let’s talk about your path forward, because that’s what this is really all about, right?
Recovery from chronic feelings of fatigue and low well-being isn’t about perfection. Let me say that again: it’s not about perfection. It’s about progress. It’s about identifying which of these four pillars are most problematic in your specific situation and creating a realistic plan to address them systematically.
Some people might need to start with lifestyle factors because their fatigue is so severe they can’t function well enough to make other changes. Others might begin with addressing psychological patterns or seeking medical evaluation for underlying conditions.
The key is an honest self-assessment and a willingness to invest in your long-term wellbeing rather than seeking immediate relief.
And you know what? That’s hard. It requires patience. It requires self-compassion. It requires accepting that some days will be better than others, and that setbacks are part of the process, not signs of failure.
Your First Step
Before you go, I want to leave you with a few simple questions. Try to answer them honestly as you reflect on your day:
- Did I feel refreshed when I woke up this morning?
- How many times did I reach for caffeine just to get through the day?
- Did I move my body today in any meaningful way?
- Did I experience more negative or positive thoughts?
- Was there a moment today that felt truly mine?
These aren’t just checkboxes. These are signals – your body’s way of telling you what it needs. You can find a full 7-Day Checklist on our website for free, and I strongly encourage you to try it. In just one week, you’ll start to see patterns emerge – patterns that can change everything.
(Download your free 7-Day Checklist below – no commitments, just curiosity and self-awareness.)
Don’t try to tackle everything at once. That’s a recipe for burnout and frustration. Instead, identify the two or three areas where you recognize the most significant problems in your life. These will likely be your highest-impact starting points.
Maybe it’s your sleep that’s really suffering. Maybe it’s the fact that you haven’t moved your body in weeks. Maybe it’s the constant mental chatter and stress. Maybe it’s your nutrition. Be honest with yourself.
And here’s the thing: you don’t have to have all the answers right now. You don’t have to have a perfect plan. You just need to start paying attention and gathering information.

Your Future Self Is Waiting
Your future self – the one who wakes up refreshed, tackles challenges with clarity, and has energy left over for the people and activities you love – is waiting for you to take that first step.
Start now. Don’t wait for the perfect moment. Because let’s be honest, the perfect moment never comes. You have to create it.
Stop guessing, start knowing.
This is Your Space Today – delivering the science-backed clarity you need every week because your health journey deserves expert guidance.
If you found value in this article, I’d really appreciate it if you’d share it with friends or family who might be struggling with similar issues. Sometimes, understanding that we’re not alone in this struggle, and that there are real, science-based explanations for what we’re experiencing – that knowledge alone can be incredibly empowering.
This article is for educational purposes only and does not constitute medical advice, diagnosis, or treatment. Always consult with your healthcare provider regarding any health concerns. You can find detailed information here.
Thank you so much for spending this time with me today. Until next time, take care of yourself. You deserve it.
Scientific References
If you’d like to explore the research behind this article, here are selected peer-reviewed studies supporting the key points discussed
- Dzakpasu, F. Q. S., Carver, A., Brakenridge, C. J., Cicuttini, F., Urquhart, D. M., Owen, N., & Dunstan, D. W. (2021). Musculoskeletal pain and sedentary behaviour in occupational and non-occupational settings: A systematic review with meta-analysis. International Journal of Behavioral Nutrition and Physical Activity, 18(1), 159. https://doi.org/10.1186/s12966-021-01191-y
- Finley CR, Chan DS, Garrison S, et al. (2018) What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018;64(11):832-840.
- Goyal, J., et al. (2024). Sedentarism and chronic health problems. PMC, PMC11427223. https://pmc.ncbi.nlm.nih.gov/articles/PMC11427223/
- Kirsch Micheletti, J., Bláfoss, R., Sundstrup, E., Bay, H., Pastre, C. M., & Andersen, L. L., et al. (2019). Association between lifestyle and musculoskeletal pain: Cross-sectional study among 10,000 adults from the general working population. BMC Musculoskeletal Disorders, 20(1), 609. https://doi.org/10.1186/s12891-019-3002-5
- Latimer, K. M., Gunther, A., & Kopec, M. (2023). Fatigue in adults: Evaluation and management. American Family Physician, 108(1), 58‑69. https://www.aafp.org/pubs/afp/issues/2023/0700/fatigue-adults.html
- Leproult, R., & Van Cauter, E. (2011). Role of sleep and sleep loss in hormonal release and metabolism. Endocrine Development, 17, 11–21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065172/
- Lurati, A. R. (2018). Health issues and injury risks associated with prolonged sitting and sedentary lifestyles. Workplace Health & Safety, 66(9), 428–436. https://doi.org/10.1177/2165079917737558
- Newton, J. L., Pairman, J., Hallsworth, K., Moore, S., Plötz, T., & Trenell, M. I. (2011). Physical activity intensity but not sedentary activity is reduced in chronic fatigue syndrome and is associated with autonomic regulation. QJM: An International Journal of Medicine, 104(8), 681–687. https://doi.org/10.1093/qjmed/hcr029
- Nollet, M., Wisden, W., & Meerlo, P. (2020). Sleep deprivation and stress: A reciprocal relationship. Interface Focus, 10(3), 20190092. https://doi.org/10.1098/rsfs.2019.0092
- Ren, Z., et al. (2025). The impact of sleep deprivation on cognitive function in healthy adults: Insights from auditory P300 and reaction time analysis. Frontiers in Neuroscience, 19, 1559969. https://doi.org/10.3389/fnins.2025.1559969
- Rogers, M., et al. (2024). The effects of sleep disruption on metabolism, hunger, and satiety, and the influence of psychosocial stress and exercise: A narrative review. Diabetes/Metabolism Research and Reviews, 40(2), e3667. https://doi.org/10.1002/dmrr.3667
- Yoon, J.‑H., Park, N.‑H., Kang, Y.‑E., Ahn, Y.‑C., Lee, E.‑J., & Son, C.‑G. (2023). The demographic features of fatigue in the general population worldwide: A systematic review and meta‑analysis. Frontiers in Public Health, 11, Article 1192121. https://www.frontiersin.org/articles/10.3389/fpubh.2023.1192121/full